Tuesday, December 17, 2013
Three weeks
Tuesday, December 10, 2013
Two weeks old
Sunday, December 8, 2013
Together
Friday, December 6, 2013
December 6
Nine days
Wednesday, December 4, 2013
8 days old - oral feedings
Monday, December 2, 2013
Briella - 6 days old
Saturday, November 30, 2013
Briella - 4 days old
Medically speaking, things are moving along slowly. Briella has been seen by most of the specialists who need to evaluate her and the prognosis seems good. The two things that we are waiting for before we can bring her home (in my understanding) is 1) her breathing needs to improve a bit - she's still having some "insucking" around the rib cage when she breaths, meaning that she's straining a bit. She also has some stridor but chances are she'll have that for a while. I still think that her breathing is stronger than Maddy's was at birth, and the doctor who was looking after Maddy agrees. 2) she is still being fed by the NG tube. She needs to start feeding orally. I'm HOPING that this will start taking place next week.
Thursday, November 28, 2013
Briella Faith
As the title of this post suggests, we have decided on a name for our little one: Briella Faith. "Briella" is a short form of the name "Gabriella" meaning "God is my strength".
Today, I will be discharged from hospital to recover from home. I'm doing very well - both physically and emotionally. The cesarean was not as painful as I'd imagined and certain aspects of the recovery are also significantly easier. When I was admitted to the hospital, I requested that I could recover in the prenatal ward rather than the postnatal ward. The prenatal ward has some postnatal patients as well, and I knew that it would be easier on me emotionally than being in the postnatal ward with 50 newborns. Thankfully they were able to accommodate my request as my hospital stay here has been so much easier than my previous two experiences!
Briella is still in the NICU. Like Maddy, her main issue is her breathing and airways. She had other medical needs such as cleft palate and clubbed feet (which are new to us, Maddy's feet are great!) But these are not what is keeping her in NICU.
It will take at least a few days or so for all the necessary specialists to see Briella and they need to consult with each other about the management plan. Although the doctor told Bernard perhaps only a few weeks, this is just a guess until we know what the plan involves...
In the meantime, Briella has started feeding through a tube, so I am pumping again. Thankfully my milk has started to come in so I'm able to meet her needs. Every time that I've seen her, she's been asleep. Since she is still on the CPAP, we are not yet able to hold her. Hopefully we can hold her soon! Also, until she is discharged, Bernard and I are the only ones able to visit her. Lana is quite upset about that, and for me, that has been the hardest thing so far :(
Please continue to pray for us, especially little Briella...
Tuesday, November 26, 2013
Welcome, baby girl!
After a lot of waiting, our third daughter (still unnamed) was born today at 1:17pm via cesarean section. She weighs 3.4kg and had apgar scores of 7 (1 minute) and 9 (5 minutes). She needed a bit of help starting to breathe due to wet lung syndrome (possibly due more to cesarean delivery than her dwarfism) and was taken quickly after birth the NICU where she was put on oxygen. Other than that, she seems healthy and strong. The doctors estimate that she may be home within 2-3 weeks which would mean she's likely to be home for Christmas! I haven't spent much time with her yet since I am still recovering from the cesarean. She looks so much like Maddy did at birth!
Thanks so much for your prayers, messages and other support. I will continue to update as we learn more.
Monday, November 25, 2013
The day before D-Day
Thursday, November 21, 2013
26 November
Maddy update
Maddy is growing well and still is extremely healthy. It has been nearly two months since we have seen the orthopedic doctors and we are still waiting for a CT appointment for her spine. I think the stress of this pregnancy (which is no where near as bad as the stress of my last pregnancy!) has taken my attention off Maddy's needs in some ways, because I'm sure I'd be more worried about it if I weren't focused on the new little one. I've figured though that the CT scan would at least give us more information about her spine and whether or not the suggested surgery is viable. Even if the suggested surgery is not viable, more information cannot be a bad thing!
Wednesday, November 20, 2013
ECV results
Tuesday, November 19, 2013
NICU - what I'd do differently
Friday, November 15, 2013
Maddy's NICU summary
Wednesday, November 13, 2013
ECV decision
- For peace in the whole situation. I'm mostly doing ok but getting a bit anxious about the delivery, recovery and hospitalisation.
- For the best possible outcome for the ECV. If she's meant to turn, that she'll turn. If cesarean is safer for her, then that she won't turn. That there will be no complications - I'd really prefer NOT to have an emergency cesarean but if that's what is best, then so be it.
- For our little girl's breathing once she is born - for her to be able to breath strongly and independently without any extra support.
Sunday, November 10, 2013
ECV or no ECV?
Sunday, November 3, 2013
Best possible outcome?
- the baby would turn and I'd have no need for a cesarean (I really don't like the sound of the recovery from that!)
- when she is born, we'll find that she has no cleft palate and can breastfeed so I don't have to think about pumping again.
- her breathing would be efficient and regular, needing no assistance such as CPAP or oxygen.
- I'd be able to bring her home from the hospital with me.
- Possible - but I'm not really holding my breath for it... Some babies, even with DD, can turn as late as right before delivery. It is rare though - but not impossible.
- I think of the above, this is the least likely. We haven't been able to see a cleft on the ultrasound, but we never saw Maddy's either. Cleft palate often goes along with a small jaw and restricted airways - and we already know she has a small jaw.
- I think this is possible - Maddy really needed minimal assistance, and I'm pretty sure that this daughter has a larger rib cage than Maddy did - so... fingers crossed!
- At times, this seems like a far off dream - I go between trying not to get my hopes up too much, and reminding myself that I need to prepare to come home alone again.
Tuesday, October 29, 2013
Delivery options
Monday, October 7, 2013
Maddy's orthopedic update
When we arrived back in Hong Kong, I saw one doctor on the spinal team. I discussed Maddy's case with him and he recommended against the casting for various reasons. I mentioned Dr Mackenzie's thoughts to him and asked if he could contact him and his response was "I could contact him but it wouldn't make me change my opinion anyway." This response bothered me - but as he was going to refer me to maybe the most senior doctor on the team, I figured I would just let it go and see what the other guy had to say.
I was really excited to meet with this senior doctor - he is very well respected, is a professor and has made some amazing and exciting contributions to spinal surgery. The appointment with him went very well, I thought.
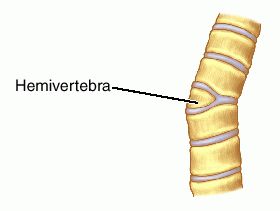
At our first appointment with the spinal team back in January of last year, a doctor there mentioned that Maddy had a hemivertebra. At that stage, it was just a "kink" and the scoliosis had not yet developed. What is a hemivertebra? Have a look at this picture:
Basically, a hemivertebra is when only half of the vertebra develops. As a result, you see this kind of a "kink" in the spine and the spine then curves into a scoliosis so that the body isn't held at this strange angle.
Since the hemivertebra had been mentioned before, I didn't question it when this professor brought it up again. Basically, his plan would be within the next 18 months or so, to remove the deformed vertebra and fuse the two vertebra either side of it together. Doing so would remove the source of the scoliosis and theoretically, it would improve the curves in Maddy's spine. He also commented that casting was not likely to be effective in the upper thoracic region where Maddy's main curves are, and that this was our best option at the current time. We planned to do a CT scan to get a better picture of the hemivertebra and to be able to prepare for probable surgery.
I left the appointment feeling quite positive - of course I dread the thought of spinal surgery, but this kind of surgery is far less major than putting rods along her entire spine, and it is a plan - I like to have a plan! I neglected to ask this doctor if he could consult with Dr Mackenzie as I thought I would go home and ask his opinion on this plan myself.
I emailed Dr Mackenzie and waited for his reply. When he wrote back, he told me that he does not believe that Maddy has a hemivertebra, that he would still recommend casting, that he would avoid surgery for now and that he would not recommend having the CT scan as he was quite sure it was not a hemivertebra anyway (it is best to avoid unnecessary CT scans as each scan contains the same level of radiation as something like 100 x-rays). He also confirmed that casting was probably not going to correct the curves in Maddy's upper spine (where her major issues are) but that it was likely to have a positive effect on her less severely curved lower spine.
It is a hard place to be, stuck between two differing opinions of two highly qualified doctors. Not knowing exactly what to do, I emailed our doctor here in Hong Kong with Dr Mackenzie's thoughts and asked if he could please consult with him as to what the best plan would be. I also had probably my biggest melt-down since I was pregnant with Maddy (can I blame pregnancy hormones again?) As a parent, I just want what is best for Maddy and sometimes it is hard to know exactly what that is. Our spinal team here are very good at what they do and they are highly specialised in the spine and in scoliosis. They don't, however, have a great amount of experience in diastrophic dysplasia. Dr Mackenzie on the other hand has maybe more experience than anyone in diastrophic dysplasia - however he deals with the whole body - spine, feet, knees, hips... I figure that if these two experts can communicate together we'd have the best of both.
Ultimately, though, Dr Mackenzie is not our doctor - he is just consulting with our doctors here. And if they (for whatever reason) choose not to avail themselves of his expertise, we cannot force them to communicate with him. I think that our doctor here may try to contact him though - I sincerely hope that he does.
After a few days and a lot of thinking, I've realised though that we still have time to figure this out. As much as I'd like to know the plan right now, the simple fact is this is still up in the air. As for casting, knowing that it will not really help her main curve that much makes it less urgent to me - I am happy for now to leave that alone.
Maddy may or may not have a hemivertebra. The CT scan definitely would help to clear that up so I think if these two experts cannot agree, we would be foolish not to proceed with the CT scan. As to what that shows and what the outcome will be there, we'll figure that out later. "Wait and see" - that seems to be the story of our life!